Introduction – Company Background
GuangXin Industrial Co., Ltd. is a specialized manufacturer dedicated to the development and production of high-quality insoles.
With a strong foundation in material science and footwear ergonomics, we serve as a trusted partner for global brands seeking reliable insole solutions that combine comfort, functionality, and design.
With years of experience in insole production and OEM/ODM services, GuangXin has successfully supported a wide range of clients across various industries—including sportswear, health & wellness, orthopedic care, and daily footwear.
From initial prototyping to mass production, we provide comprehensive support tailored to each client’s market and application needs.
At GuangXin, we are committed to quality, innovation, and sustainable development. Every insole we produce reflects our dedication to precision craftsmanship, forward-thinking design, and ESG-driven practices.
By integrating eco-friendly materials, clean production processes, and responsible sourcing, we help our partners meet both market demand and environmental goals.


Core Strengths in Insole Manufacturing
At GuangXin Industrial, our core strength lies in our deep expertise and versatility in insole and pillow manufacturing. We specialize in working with a wide range of materials, including PU (polyurethane), natural latex, and advanced graphene composites, to develop insoles and pillows that meet diverse performance, comfort, and health-support needs.
Whether it's cushioning, support, breathability, or antibacterial function, we tailor material selection to the exact requirements of each project-whether for foot wellness or ergonomic sleep products.
We provide end-to-end manufacturing capabilities under one roof—covering every stage from material sourcing and foaming, to precision molding, lamination, cutting, sewing, and strict quality control. This full-process control not only ensures product consistency and durability, but also allows for faster lead times and better customization flexibility.
With our flexible production capacity, we accommodate both small batch custom orders and high-volume mass production with equal efficiency. Whether you're a startup launching your first insole or pillow line, or a global brand scaling up to meet market demand, GuangXin is equipped to deliver reliable OEM/ODM solutions that grow with your business.


Customization & OEM/ODM Flexibility
GuangXin offers exceptional flexibility in customization and OEM/ODM services, empowering our partners to create insole products that truly align with their brand identity and target market. We develop insoles tailored to specific foot shapes, end-user needs, and regional market preferences, ensuring optimal fit and functionality.
Our team supports comprehensive branding solutions, including logo printing, custom packaging, and product integration support for marketing campaigns. Whether you're launching a new product line or upgrading an existing one, we help your vision come to life with attention to detail and consistent brand presentation.
With fast prototyping services and efficient lead times, GuangXin helps reduce your time-to-market and respond quickly to evolving trends or seasonal demands. From concept to final production, we offer agile support that keeps you ahead of the competition.
Quality Assurance & Certifications
Quality is at the heart of everything we do. GuangXin implements a rigorous quality control system at every stage of production—ensuring that each insole meets the highest standards of consistency, comfort, and durability.
We provide a variety of in-house and third-party testing options, including antibacterial performance, odor control, durability testing, and eco-safety verification, to meet the specific needs of our clients and markets.
Our products are fully compliant with international safety and environmental standards, such as REACH, RoHS, and other applicable export regulations. This ensures seamless entry into global markets while supporting your ESG and product safety commitments.
ESG-Oriented Sustainable Production
At GuangXin Industrial, we are committed to integrating ESG (Environmental, Social, and Governance) values into every step of our manufacturing process. We actively pursue eco-conscious practices by utilizing eco-friendly materials and adopting low-carbon production methods to reduce environmental impact.
To support circular economy goals, we offer recycled and upcycled material options, including innovative applications such as recycled glass and repurposed LCD panel glass. These materials are processed using advanced techniques to retain performance while reducing waste—contributing to a more sustainable supply chain.
We also work closely with our partners to support their ESG compliance and sustainability reporting needs, providing documentation, traceability, and material data upon request. Whether you're aiming to meet corporate sustainability targets or align with global green regulations, GuangXin is your trusted manufacturing ally in building a better, greener future.
Let’s Build Your Next Insole Success Together
Looking for a reliable insole manufacturing partner that understands customization, quality, and flexibility? GuangXin Industrial Co., Ltd. specializes in high-performance insole production, offering tailored solutions for brands across the globe. Whether you're launching a new insole collection or expanding your existing product line, we provide OEM/ODM services built around your unique design and performance goals.
From small-batch custom orders to full-scale mass production, our flexible insole manufacturing capabilities adapt to your business needs. With expertise in PU, latex, and graphene insole materials, we turn ideas into functional, comfortable, and market-ready insoles that deliver value.
Contact us today to discuss your next insole project. Let GuangXin help you create custom insoles that stand out, perform better, and reflect your brand’s commitment to comfort, quality, and sustainability.
🔗 Learn more or get in touch:
🌐 Website: https://www.deryou-tw.com/
📧 Email: shela.a9119@msa.hinet.net
📘 Facebook: facebook.com/deryou.tw
📷 Instagram: instagram.com/deryou.tw
Memory foam pillow OEM factory Taiwan
Are you looking for a trusted and experienced manufacturing partner that can bring your comfort-focused product ideas to life? GuangXin Industrial Co., Ltd. is your ideal OEM/ODM supplier, specializing in insole production, pillow manufacturing, and advanced graphene product design.
With decades of experience in insole OEM/ODM, we provide full-service manufacturing—from PU and latex to cutting-edge graphene-infused insoles—customized to meet your performance, support, and breathability requirements. Our production process is vertically integrated, covering everything from material sourcing and foaming to molding, cutting, and strict quality control.Vietnam graphene product OEM service
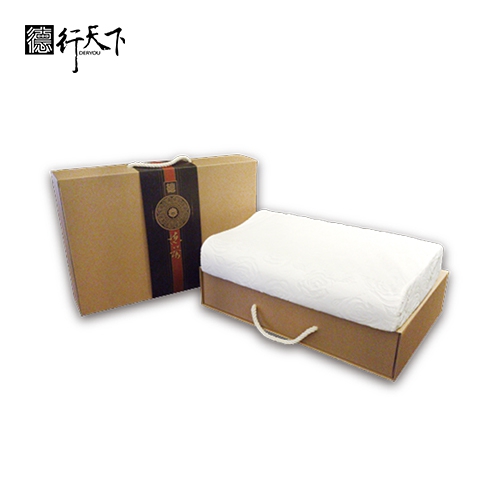
Beyond insoles, GuangXin also offers pillow OEM/ODM services with a focus on ergonomic comfort and functional innovation. Whether you need memory foam, latex, or smart material integration for neck and sleep support, we deliver tailor-made solutions that reflect your brand’s values.
We are especially proud to lead the way in ESG-driven insole development. Through the use of recycled materials—such as repurposed LCD glass—and low-carbon production processes, we help our partners meet sustainability goals without compromising product quality. Our ESG insole solutions are designed not only for comfort but also for compliance with global environmental standards.Taiwan insole ODM service provider
At GuangXin, we don’t just manufacture products—we create long-term value for your brand. Whether you're developing your first product line or scaling up globally, our flexible production capabilities and collaborative approach will help you go further, faster.Latex pillow OEM production in Thailand
📩 Contact us today to learn how our insole OEM, pillow ODM, and graphene product design services can elevate your product offering—while aligning with the sustainability expectations of modern consumers.Taiwan insole ODM for global brands
The new technology correctly identified 99% of confirmed bacterial sepsis cases, 92% of confirmed viral sepsis cases, and predicted sepsis in 74% of clinically suspected but undiagnosed cases. Remarkable accuracy – a sepsis diagnosis tool combines genetic sequencing with analysis of patients’ immune responses. According to estimates, sepsis—a condition in which the immune system overreacts to an infection—causes 20% of fatalities worldwide and somewhere between 20 and 50% of hospital deaths in the United States each year. Despite its frequency and severity, the condition is challenging to identify and effectively treat. Chaz Langelier, M.D., Ph.D., an associate professor of medicine in UCSF’s Division of Infectious Diseases and a CZ Biohub Investigator, is senior author of a study describing a remarkably accurate diagnostic tool for sepsis. Credit: CZ Biohub The disease can result in reduced blood flow to essential organs, widespread inflammation, and irregular blood clotting. As a result, sepsis may result in shock, organ failure, and death if it is not promptly diagnosed and treated. However, determining which pathogen is causing sepsis or if an infection is present in the bloodstream or elsewhere in the body may be challenging. Additionally, it may be tough to evaluate whether a patient really has an infection in many cases with symptoms that resemble sepsis. Researchers from the Chan Zuckerberg Biohub, the Chan Zuckerberg Initiative, and the University of California, San Francisco have now created a novel diagnostic method that employs machine learning to analyze advanced genomics data from both the host and the pathogen to recognize and predict sepsis cases. The method is reportedly unexpectedly accurate and has the potential to far outperform present diagnostic skills. The researchers’ findings were recently published in the journal Nature Microbiology. “Sepsis is one of the top 10 public health issues facing humanity,” said senior author Chaz Langelier, M.D., Ph.D., an associate professor of medicine in UCSF’s Division of Infectious Diseases and a CZ Biohub Investigator. “One of the key challenges with sepsis is diagnosis. Existing diagnostic tests are not able to capture the dual-sided nature of the disease – the infection itself and the host’s immune response to the infection.” Current sepsis diagnostics focus on detecting bacteria by growing them in culture, a process that is “essential for appropriate antibiotic therapy, which is critical for sepsis survival,” according to the researchers behind the new method. But culturing these pathogens is time-consuming and doesn’t always correctly identify the bacterium that is causing the infection. Similarly, for viruses, PCR tests can detect that viruses are infecting a patient but don’t always identify the particular virus that’s causing sepsis. “This results in clinicians being unable to identify the cause of sepsis in an estimated 30 to 50% of cases,” Langelier said. “This also leads to a mismatch in terms of the antibiotic treatment and the pathogen causing the problem.” In the absence of a definitive diagnosis, doctors often prescribe a cocktail of antibiotics in an effort to stop the infection, but the overuse of antibiotics has led to increased antibiotic resistance worldwide. “As physicians, we never want to miss a case of infection,” said Carolyn Calfee, M.D., M.A.S., a professor of medicine and anesthesia at UCSF and co-senior author of the new study. “But if we had a test that could help us accurately determine who doesn’t have an infection, then that could help us limit antibiotic use in those cases, which would be really good for all of us.” Eliminating Ambiguity The researchers analyzed whole blood and plasma samples from more than 350 critically ill patients who had been admitted to UCSF Medical Center or the Zuckerberg San Francisco General Hospital between 2010 and 2018. But rather than relying on cultures to identify pathogens in these samples, a team led by CZ Biohub scientists Norma Neff, Ph.D., and Angela Pisco, Ph.D., instead used metagenomic next-generation sequencing (mNGS). This method identifies all the nucleic acids or genetic data present in a sample, then compares those data to reference genomes to identify the microbial organisms present. This technique allows scientists to identify genetic material from entirely different kingdoms of organisms – whether bacteria, viruses, or fungi – that are present in the same sample. However, detecting and identifying the presence of a pathogen alone isn’t enough for accurate sepsis diagnosis, so the Biohub researchers also performed transcriptional profiling – which quantifies gene expression – to capture the patient’s response to infection. Next, they applied machine learning to the mNGS and transcriptional data to distinguish between sepsis and other critical illnesses and thus confirm the diagnosis. Katrina Kalantar, Ph.D., a lead computational biologist at CZI and co-first author of the study, created an integrated host-microbe model trained on data from patients in whom either sepsis or non-infectious systemic inflammatory illnesses had been established, which enabled sepsis diagnosis with very high accuracy. “We developed the model by looking at a bunch of metagenomics data alongside results from traditional clinical tests,” Kalantar explained. To start, the researchers identified changes in gene expression between patients with confirmed sepsis and non-infectious systemic inflammatory conditions that appear clinically similar, then used machine learning to identify the genes that could best predict those changes. The researchers found that when traditional bacterial culture identified a sepsis-causing pathogen, there was usually an overabundance of genetic material from that pathogen in the corresponding plasma sample analyzed by mNGS. With that in mind, Kalantar programmed the model to identify organisms present in disproportionately high abundance compared to other microbes in the sample, and to then compare those to a reference index of well-known sepsis-causing microbes. “In addition to that, we also noted any viruses that were detected, even if they were at lower levels, because those really shouldn’t be there,” Kalantar explained. “With this relatively straightforward set of rules, we were able to do pretty well.” ‘Almost Perfect’ Performance The researchers found that the mNGS method and their corresponding model worked better than expected: They were able to identify 99% of confirmed bacterial sepsis cases, 92% of confirmed viral sepsis cases, and were able to predict sepsis in 74% of clinically suspected cases that hadn’t been definitively diagnosed. “We were expecting good performance, or even great performance, but this was almost perfect,” said Lucile Neyton, Ph.D., a postdoctoral researcher in the Calfee lab and co-first author of the study. “By using this approach, we get a pretty good idea of what is causing the disease, and we know with relatively high confidence if a patient has sepsis or not.” The team was also excited to discover that they could use this combined host-response and microbe detection method to diagnose sepsis using plasma samples, which are routinely collected from most patients as part of standard clinical care. “The fact that you can actually identify sepsis patients from this widely available, easy-to-collect sample type has big implications in terms of practical utility,” Langelier said. The idea for the work stemmed from a previous Proceedings of the National Academy of Sciences study by Langelier, Kalantar, Calfee, UCSF researcher and CZ Biohub President Joe DeRisi, Ph.D., and their colleagues, in which they used mNGS to effectively diagnose lower respiratory tract infections in critically ill patients. Because the method worked so well, “we wanted to see if the same type of approach could work in the context of sepsis,” said Kalantar. Broader Implications The team hopes to build upon this successful diagnostic technique by developing a model that can also predict antibiotic resistance from pathogens detected with this method. “We’ve had some success doing that for respiratory infections, but no one has come up with a good approach for sepsis,” Langelier said. Furthermore, the researchers hope to eventually be able to predict outcomes of patients with sepsis, “such as mortality or length of stay in the hospital, which would provide key information that would allow clinicians to better care for their patients and match resources to the patients who need them the most,” Langelier said. “There’s a lot of potential for novel sequencing approaches such as this to help us more precisely identify the causes of a patient’s critical illness,” added Calfee. “If we can do that, it’s the first step towards precision medicine and understanding what’s going on at an individual patient level.” References: “Integrated host-microbe plasma metagenomics for sepsis diagnosis in a prospective cohort of critically ill adults” by Katrina L. Kalantar, Lucile Neyton, Mazin Abdelghany, Eran Mick, Alejandra Jauregui, Saharai Caldera, Paula Hayakawa Serpa, Rajani Ghale, Jack Albright, Aartik Sarma, Alexandra Tsitsiklis, Aleksandra Leligdowicz, Stephanie A. Christenson, Kathleen Liu, Kirsten N. Kangelaris, Carolyn Hendrickson, Pratik Sinha, Antonio Gomez, Norma Neff, Angela Pisco, Sarah B. Doernberg, Joseph L. Derisi, Michael A. Matthay, Carolyn S. Calfee and Charles R. Langelier, 20 October 2022, Nature Microbiology. DOI: 10.1038/s41564-022-01237-2 “Integrating host response and unbiased microbe detection for lower respiratory tract infection diagnosis in critically ill adults” by Charles Langelier, Katrina L. Kalantar, Farzad Moazed, Michael R. Wilson, Emily D. Crawford, Thomas Deiss, Annika Belzer, Samaneh Bolourchi, Saharai Caldera, Monica Fung, Alejandra Jauregui, Katherine Malcolm, Amy Lyden, Lillian Khan, Kathryn Vessel, Jenai Quan, Matt Zinter, Charles Y. Chiu, Eric D. Chow, Jenny Wilson, Steve Miller, Michael A. Matthay, Katherine S. Pollard, Stephanie Christenson, Carolyn S. Calfee and Joseph L. DeRisi, 27 November 2018, Proceedings of the National Academy of Sciences. DOI: 10.1073/pnas.1809700115 The study was funded by the National Heart, Lung, and Blood Institute and the Chan Zuckerberg Biohub.
Illustration of the cyanobacterial thylakoid membrane. Credit: Luning Liu et al. A new study conducted by the researchers at the University of Liverpool reveals how the ancient photosynthetic organisms – cyanobacteria – evolve their photosynthetic machinery and organize their photosynthetic membrane architecture for the efficient capture of solar light and energy transduction. Oxygenic photosynthesis, carried out by plants, algae, and cyanobacteria, produces energy and oxygen for life on Earth and is arguably the most important biological process. Cyanobacteria are among the earliest phototrophs that can perform oxygenic photosynthesis and make significant contributions to the Earth’s atmosphere and primary production. Light-dependent photosynthetic reactions are performed by a set of photosynthetic complexes and molecules accommodated in the specialized cell membranes, called thylakoid membranes. While some studies have reported the structures of photosynthetic complexes and how they perform photosynthesis, researchers still had little understanding about how native thylakoid membranes are built and further developed to become a functional entity in cyanobacterial cells. The research team, led by Professor Luning Liu from the University’s Institute of Systems, Molecular and Integrative Biology, developed a method to control the formation of thylakoid membranes during cell growth and used state-of-the-art proteomics and microscopic imaging to characterize the stepwise maturation process of thylakoid membranes. Their results are published in the journal Nature Communications. “We are really thrilled about the findings,” said Professor Liu. “Our research draws a picture about how phototrophs generate and then develop their photosynthetic membranes, and how different photosynthetic components are incorporated and located in the thylakoid membrane to perform efficient photosynthesis – a long-standing question in this field.” The first author of the study, Dr. Tuomas Huokko, said: “We find that the newly synthesized thylakoid membranes emerge between the peripheral cell membrane, termed the plasma membrane, and the pre-existing thylakoid layer. By detecting the protein compositions and photosynthetic activities during the thylakoid development process, we also find that photosynthetic proteins are well controlled in space and time to evolve and assemble into the thylakoid membranes.” The new research shows that the cyanobacterial thylakoid membrane is a truly dynamic biological system and can adapt rapidly to environmental changes during bacterial growth. In thylakoids, photosynthetic proteins can diffuse from one position to another and form functional “protein islands” to work together for high photosynthetic efficiency. “Since cyanobacteria perform plant-like photosynthesis, the knowledge gained from cyanobacteria thylakoid membranes can be extended to plant thylakoids,” added Professor Liu. “Understanding how the natural photosynthetic machinery is evolved and regulated in phototrophs is vital for tuning and enhancing photosynthetic performance. This offers solutions to sustainably improve crop plant photosynthesis and yields, in the context of climate change and growing population. Our research may also benefit the bioinspired design and generation of artificial photosynthetic devices for efficient electron transfer and bioenergy production.” Reference: “Probing the biogenesis pathway and dynamics of thylakoid membranes” by Tuomas Huokko, Tao Ni, Gregory F. Dykes, Deborah M. Simpson, Philip Brownridge, Fabian D. Conradi, Robert J. Beynon, Peter J. Nixon, Conrad W. Mullineaux, Peijun Zhang and Lu-Ning Liu, 9 June 2021, Nature Communications. DOI: 10.1038/s41467-021-23680-1 The research was carried out in collaboration with the University’s Centre for Proteome Research, Centre for Cell Imaging, and Biomedical Electron Microscopy Unit, as well as with researchers from University of Oxford, Queen Mary University of London, and Imperial College London. The research was funded by the BBSRC, Royal Society, Wellcome Trust, and Leverhulme Trust.
The researchers took this image of a tumor using immunofluorescence, a technique that allows them to stain tissue sections with fluorescently-labeled antibodies or dyes. Blue indicates the cell nuclei, green signifies tumor regions, and red is a marker for T cells. Credit: Elen Torres-Mejia Researchers decipher when and why immune cells fail to respond to immunotherapy, suggesting that T cells need a different kind of prodding to re-engage the immune response. Non-small cell lung cancer (NSCLC) is the most common type of lung cancer in humans. Some patients with NSCLC receive a therapy called immune checkpoint blockade (ICB) that helps kill cancer cells by reinvigorating a subset of immune cells called T cells, which are “exhausted” and have stopped working. However, only about 35% of NSCLC patients respond to ICB therapy. Stefani Spranger’s lab at the MIT Department of Biology explores the mechanisms behind this resistance, with the goal of inspiring new therapies to better treat NSCLC patients. In a new study published on October 29 in Science Immunology, a team led by Spranger lab postdoc Brendan Horton revealed what causes T cells to be non-responsive to ICB — and suggests a possible solution. Scientists have long thought that the conditions within a tumor were responsible for determining when T cells stop working and become exhausted after being overstimulated or working for too long to fight a tumor. That’s why physicians prescribe ICB to treat cancer — ICB can invigorate the exhausted T cells within a tumor. However, Horton’s new experiments show that some ICB-resistant T cells stop working before they even enter the tumor. These T cells are not actually exhausted, but rather they become dysfunctional due to changes in gene expression that arise early during the activation of a T cell, which occurs in lymph nodes. Once activated, T cells differentiate into certain functional states, which are distinguishable by their unique gene expression patterns. The notion that the dysfunctional state that leads to ICB resistance arises before T cells enter the tumor is quite novel, says Spranger, the Howard S. and Linda B. Stern Career Development Professor, a member of the Koch Institute for Integrative Cancer Research, and the study’s senior author. “We show that this state is actually a preset condition, and that the T cells are already non-responsive to therapy before they enter the tumor,” she says. As a result, she explains, ICB therapies that work by reinvigorating exhausted T cells within the tumor are less likely to be effective. This suggests that combining ICB with other forms of immunotherapy that target T cells differently might be a more effective approach to help the immune system combat this subset of lung cancer. In order to determine why some tumors are resistant to ICB, Horton and the research team studied T cells in murine models of NSCLC. The researchers sequenced messenger RNA from the responsive and non-responsive T cells in order to identify any differences between the T cells. Supported in part by the Koch Institute Frontier Research Program, they used a technique called Seq-Well, developed in the lab of fellow Koch Institute member J. Christopher Love, the Raymond A. (1921) and Helen E. St. Laurent Professor of Chemical Engineering and a co-author of the study. The technique allows for the rapid gene expression profiling of single cells, which permitted Spranger and Horton to get a very granular look at the gene expression patterns of the T cells they were studying. Seq-Well revealed distinct patterns of gene expression between the responsive and non-responsive T cells. These differences, which are determined when the T cells assume their specialized functional states, may be the underlying cause of ICB resistance. Now that Horton and his colleagues had a possible explanation for why some T cells did not respond to ICB, they decided to see if they could help the ICB-resistant T cells kill the tumor cells. When analyzing the gene expression patterns of the non-responsive T cells, the researchers had noticed that these T cells had a lower expression of receptors for certain cytokines, small proteins that control immune system activity. To counteract this, the researchers treated lung tumors in murine models with extra cytokines. As a result, the previously non-responsive T cells were then able to fight the tumors — meaning that the cytokine therapy prevented, and potentially even reversed, the dysfunctionality. Administering cytokine therapy to human patients is not currently safe, because cytokines can cause serious side effects as well as a reaction called a “cytokine storm,” which can produce severe fevers, inflammation, fatigue, and nausea. However, there are ongoing efforts to figure out how to safely administer cytokines to specific tumors. In the future, Spranger and Horton suspect that cytokine therapy could be used in combination with ICB. “This is potentially something that could be translated into a therapeutic that could increase the therapy response rate in non-small cell lung cancer,” Horton says. Spranger agrees that this work will help researchers develop more innovative cancer therapies, especially because researchers have historically focused on T cell exhaustion rather than the earlier role that T cell functional states might play in cancer. “If T cells are rendered dysfunctional early on, ICB is not going to be effective, and we need to think outside the box,” she says. “There’s more evidence, and other labs are now showing this as well, that the functional state of the T cell actually matters quite substantially in cancer therapies.” To Spranger, this means that cytokine therapy “might be a therapeutic avenue” for NSCLC patients beyond ICB. Jeffrey Bluestone, the A.W. and Mary Margaret Clausen Distinguished Professor of Metabolism and Endocrinology at the University of California-San Francisco, who was not involved with the paper, agrees. “The study provides a potential opportunity to ‘rescue’ immunity in the NSCLC non-responder patients with appropriate combination therapies,” he says. This research was funded by the Pew-Stewart Scholars for Cancer Research, the Ludwig Center for Molecular Oncology, the Koch Institute Frontier Research Program through the Kathy and Curt Mable Cancer Research Fund, and the National Cancer Institute.
DVDV1551RTWW78V
Taiwan neck support pillow OEM 》flexible, experienced, and ready to support your growthIndonesia pillow OEM manufacturer 》delivering product excellence through every detailIndonesia custom neck pillow ODM 》helping brands deliver comfort and performance
下一則: Customized sports insole ODM China 》the ideal part
限會員,要發表迴響,請先登入


